 Bill “Moley” Mohlenbrock MD, FACS ‘61 has done many interesting things in his life… member of the Illini Varsity Basketball team, married Betty Burch, Chi Omega ’62 – the Illini Homecoming Queen, served as a Naval flight surgeon aboard the aircraft carrier, USS Yorktown during the Vietnam War, completed an orthopedic residency at the University of California, San Diego, served as assistant clinical professor since 1973, and practiced orthopedic surgery for more than 25 years at Scripps Memorial Hospital in La Jolla, CA. He and Betty raised a wonderful daughter Kem, who has blessed them with four grandkids. Any of these activities would make for a fascinating interview and many of Bill’s peers are content to settle into retirement with a lot of golf and some travel. However, Bill hasn’t slowed a bit. He continues to recognize new challenges using his medical background, new technologies and passion for objectively assessing medical value, which is both quality and costs. A company he founded in 1983, now known as Verras Ltd., assists hospitals and physicians with improving their clinical quality and cost efficiencies. Self-insured employers also use the information to control healthcare costs by directing their employees to the highest quality most cost efficient providers. Recent changes in the Affordable Care Act allow physicians and hospitals to share in net-savings, if their quality of care is improved. Verras’ data provides the medical outcomes to demonstrate improvements as well as the objective and transparent clinical information with which to distribute the dollars between the hospital and its physicians – an indispensible component of any market-based healthcare solution.
Bill “Moley” Mohlenbrock MD, FACS ‘61 has done many interesting things in his life… member of the Illini Varsity Basketball team, married Betty Burch, Chi Omega ’62 – the Illini Homecoming Queen, served as a Naval flight surgeon aboard the aircraft carrier, USS Yorktown during the Vietnam War, completed an orthopedic residency at the University of California, San Diego, served as assistant clinical professor since 1973, and practiced orthopedic surgery for more than 25 years at Scripps Memorial Hospital in La Jolla, CA. He and Betty raised a wonderful daughter Kem, who has blessed them with four grandkids. Any of these activities would make for a fascinating interview and many of Bill’s peers are content to settle into retirement with a lot of golf and some travel. However, Bill hasn’t slowed a bit. He continues to recognize new challenges using his medical background, new technologies and passion for objectively assessing medical value, which is both quality and costs. A company he founded in 1983, now known as Verras Ltd., assists hospitals and physicians with improving their clinical quality and cost efficiencies. Self-insured employers also use the information to control healthcare costs by directing their employees to the highest quality most cost efficient providers. Recent changes in the Affordable Care Act allow physicians and hospitals to share in net-savings, if their quality of care is improved. Verras’ data provides the medical outcomes to demonstrate improvements as well as the objective and transparent clinical information with which to distribute the dollars between the hospital and its physicians – an indispensible component of any market-based healthcare solution.
With ObamaCare and healthcare in general so much in the news these days, I thought that Bill could help sort out the hype from the reality in this debate.
Bill, first, what prompted you to get into medicine? The Illio Yearbook lists your major, as Zoology – is that accurate?
Yes, today’s pre-med students have many choices in majors; however, my generation’s options were essentially limited to zoology, chemistry, or physics. I enjoyed zoology the most, which included subjects like anatomy and embryology. I ended up with minors in chemistry and physics.
Can you give us some background on your medical career?
My background is straightforward – I always wanted to be a physician. This was advantageous because my academic energies at Illinois were focused on science and getting into medical school. My father was an eye, ear, nose and throat doctor in Murphysboro and I observed and admired the relationship he formed with his patients. Athletics significantly influenced my interest in pursuing orthopedic surgery.
What do you like best about medical practice and what are some of the biggest challenges?
What I like best about medical practice is the bond that is created between the patient and physician. I’ve found nothing in the business world that is as rewarding or comparable to this intimate relationship. The biggest challenge is how our profession and political structure can preserve that relationship while controlling the costs of healthcare.
How has the surgeon’s role changed over the course of your career? What are some of the factors that have led to better care for patients?
Surgeons’ roles have rapidly changed in response to technologic innovations. Laparoscopic (abdominal) and arthroscopic (joint) surgeries allow limited surgical exposures, which greatly reduce postoperative discomfort for the patient and shorten hospitalizations. Radiologic advances in diagnostics, such as MRI, improve surgical precision, while radiologic cancer treatments reduce the need for more radical surgeries – all of which benefit patients.
What are some of the factors that have led to less desirable outcomes?
Certainly the rising cost of care is the most widely recognized undesirable outcome. Expensive new technologies, compliance with government regulations and the insulation by third-party payers of patients from the costs of their care has resulted in patients’ demands “that no expense should be spared”. The overuse of resources because of physicians’ and hospitals’ unrecognized inefficiencies and their fears of medical malpractice suits are also significant cost drivers.
I’m concerned that selective taxation on devices, a rather new phenomenon, will stifle medical innovations. Also, excessive risk-aversion by FDA to acceptance of new medications will create undesirable outcomes, such as we’re presently seeing in the declining number of antibiotics coming onto the market
You have started a number of companies, which are focused on improving patient care on a broader scale. What prompted you to approach healthcare in this way?
I’ve always felt that solving fundamental problems could have the greatest impact for improving healthcare quality and delivery – and the lack of quality documentation is the fundamental issue. Verras LLC is about defining and improving medical quality by assisting physicians with reducing variations in their clinical and financial outcomes. Physicians’ ordering pens control 75% to 85% of all inpatient costs and almost 100% in their offices. We help physicians by using each doctor’s own data to identify his/her best-demonstrated performances and then use techniques to replicate their superior practice patterns.
If purchasers of healthcare are unable to identify and direct patients to the highest quality and most efficient hospitals and physicians, they will be forced to continue contracting on the basis of price. Price is the primary metric used by third party payers; but price has no meaning without a measure of the quality of service or product being purchased in healthcare or any other industry.
The second fundamental problem involves the lack of information interoperability that enables medical data to be rapidly and securely shared between clinicians and first-responder personnel. Medical and public safety data are siloed in thousands of disparate databases that inhibit the flow of medical information needed to treat patients at the point of care. I founded Crossflo Inc. in 1992 in order to facilitate secure data exchanges between these databases by utilizing data sharing standards and techniques that requires little or no manual programming.
Are these technologies making a difference?
Yes, but we’ve a long, long way to go. Verras is currently working with physicians in a number of hospitals across the country where we’ve documented millions of dollars of savings per facility per year. In the early ‘90’s, at the request of the four largest, self-insured Cincinnati employers, 14 hospitals used the technologies and saved well over $200 Million in 2 years, as reported in the Wall Street Journal. But physicians were legally prohibited from sharing in the saving that they produced. Under the ObamaCare (ACA) legislation, hospitals and physicians can now share in these savings and Verras is in the process of setting up mechanisms to encourage these market-based incentives for the benefit of other self-insured employers.
Crossflo Data Exchange technology is being used to move first-responder data throughout local and state police in New Jersey as well as sharing their secure data with the FBI. Medicare (CMS) has also recently begun using Crossflo’s technology for its data sharing needs. We’re excited by the prospects of these applications, but only time will tell as to the magnitude of their economic impacts.
You had an opportunity to meet President Obama and discuss your ideas face-to-face. What was your advice to the President? Was he open to your ideas? What was the result? What are some of your observations after the experience of talking directly with the President?
One-on-one, he is very engaging, especially after I mentioned our common Illinois backgrounds and love of basketball. The intent of my meeting with the President was to inform him of the importance of helping physicians modify their clinical practices to improve quality and impress upon him the importance of that portion of the ACA law that allows for physicians and hospitals to share net-saving – if they objectively improve clinical and financial outcomes. He asked good questions, was definitely engaged and through, Reggie Love, his right-hand man (and member of the Nat. Champion Duke Basketball team 2001), I was given access to numerous individuals within the White House and HHS who wrote the law. The Presidential meeting very helpful to me and definitely worth the effort.
ObamaCare has been through many iterations… or at least the public perception of what was promised and what is being delivered does not seem to be consistent. What is your view on the program as a whole?
I, along with many others, believe that insuring patients with pre-existing conditions and those without insurance makes a great deal of ethical and financial sense. The President seemed very sincere in these regards, but as hard as I’ve tried to understand what he and the authors told me and what the law states, I can’t for the life of me understand how it can work as it now stands – and that is aside from the initial problems with the website. I think the President’s inconsistencies will seriously impair his ability to successfully promote the ACA as America’s best solution and I hope the single payer option will be taken off the table.
What do you view as the positive aspects of the program?
The ACA has elevated the need to protect patients with pre-existing conditions and those without insurance to the forefront of issues that must be solved or at least ameliorated – and these are positives. But I think they are best addressed though market-based solutions with quality-based incentives, such as the ability for hospitals and physicians to share in net saving. As I told the President, this particular change in the law aligns providers’ incentives and is an excellent step in the right direction.
What are the aspects that are not going to have their intended consequences?
Three things that are most destructive in my view are the predictable cost accelerations and the disincentives for physicians’ participation. The number of Medicaid enrollees will swamp state budgets, cause significant decreased reimbursements for providers, which will lead to decrease access to physicians who simply can’t treat patients at the expected levels of declining reimbursements. The third, and possibly most pernicious unintended consequence is the loss of individuals’ privacy.
Do you think that broader adoption of some of the concepts offered by your company could make an impact?
Irrespective of my personal views and technologies, US healthcare must progress to a true competitive model, which by the way, we have never had due to the lack of quality definitions. To move in that direction, self-insured employers should elect to selectively direct contract with providers on the basis of superior outcomes. Likewise, state governments can incentivize hospitals and physicians by rewarding those enterprises that document improving quality and cost efficiencies. (This could alleviate some of the draconian financial cuts to providers and incentivize them to continue taking care of patients with minimal [Medicaid] or no coverage. It also has the benefit of cutting out or minimizing the impact of insurance companies.) Self-insured employers and state governments have the power to implement value-based healthcare purchasing, now that we have transparent, objective and reliable metrics of quality. These initiatives should begin immediately.
What changes would you recommend?
First we must have third-party insurers competing across state lines to take advantage of value-based healthcare purchasing. Individuals should enjoy the same tax-exempt status for medical expenses as corporations. High deductible Health Saving Accounts (HSAs) coupled with catastrophic insurance plans put purchasing decisions where they belong – in the hands of patients and their families, who should retain unspent dollars for future care. States, not the federal government, should implement malpractice reforms that support patients who have experienced true malpractice misadventures but limit the unconscionably large awards based on pain and suffering. Risk pools for patients with preconditions and private insurance vouchers for Medicare patients are only a couple of additional innovations that should be considered.
What do you predict will happen with the program over the next five years?
As Yogi Berra said, “making predictions is difficult, particularly about the future” – and I add in this case, hazardous. Even more difficult is making changes to existing laws, but I think the ACA in its present form will not survive. I believe young people, who voted for President Obama in great numbers, will actually lead the movement away from the ACA. This is because they will not only find themselves shouldering our humongous national debt, but under the law will be forced to pay for health insurance they neither desire nor need, in order to subsidize the elderly who consume ever-increasing amounts of care. I also believe we’ll move back toward a more market based approach with private insurance. However, this appropriate redirection will not be adequate unless private and public purchasers, including patients, have the information they need to purchase healthcare on the basis of objective measures of value. Price-based purchasing has been the hallmark of third-party payers and must be supplanted by value-based healthcare purchasing.
We have many brothers in the medical profession in our alumni network. What recommendations do you have to them to best adapt to the changes being made to their world?
In my personal journey, I have moved from taking care of individual patients, which I loved, to using clinical data to assist hospitals and physicians in their struggles to keep abreast of clinical as well as political changes, which I also love. I’ve straddled both sides of the clinical and business fence and I believe that our profession is the most noble and gratifying of all endeavors. In spite of everything, I absolutely believe the practice of medicine is a wonderful way to positively impact people’s lives and remains a great way to make a living – nothing compares.
What recommendations do you have for our undergraduate members who are interested in a career in medicine?
Our oldest grandson Brock, enters his first year of college next year and says he wants to practice medicine, maybe even be an orthopedic surgeon. To him and all other young people to want to make a positive difference with their lives and create a secure means of making a living for themselves and their future families – there is no better way.
OK… I have to ask about your ATO time…. what are some of your favorite memories from your undergraduate years?
 The ATOs of Gamma Zeta took this Southern Illinois hick under their wings, gave him a home away from Murphysboro, provided a family with Judeo-Christian values and lifelong friends. My ATO brothers set me on my path. (The only sorority exchange I can remember attending because of basketball practice, was the Chi O exchange where I saw this long-legged beauty who is now my wife of 49 years. Of course it was her intellect that was the attraction.) My other positive memories drift back to basketball. I was the only member of my freshman basketball team to play all four years at Illinois. Bill Small ’63 may have Illinois’ free-throw percentage record, but I have the all Big Ten record for splinters in my gluteus maximus from time on the bench. Not particularly awe-inspiring, but the dean of St. Louis University Medical School said during my interview, that “because you were able to maintain these grades and a Big 10 basketball schedule, you’ll do fine in this medical school – you’re hired”.
The ATOs of Gamma Zeta took this Southern Illinois hick under their wings, gave him a home away from Murphysboro, provided a family with Judeo-Christian values and lifelong friends. My ATO brothers set me on my path. (The only sorority exchange I can remember attending because of basketball practice, was the Chi O exchange where I saw this long-legged beauty who is now my wife of 49 years. Of course it was her intellect that was the attraction.) My other positive memories drift back to basketball. I was the only member of my freshman basketball team to play all four years at Illinois. Bill Small ’63 may have Illinois’ free-throw percentage record, but I have the all Big Ten record for splinters in my gluteus maximus from time on the bench. Not particularly awe-inspiring, but the dean of St. Louis University Medical School said during my interview, that “because you were able to maintain these grades and a Big 10 basketball schedule, you’ll do fine in this medical school – you’re hired”.
Who were some of your best friends in the house?
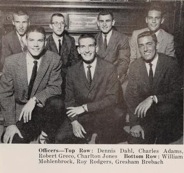
That is really tough, there were so many. Charlie Younger and I roomed together for a couple of years, Pete Fernandes was instrumental in my becoming an ATO, Denny Schlemmer and I spent hours in the chapter room studying and Dick George dragged me through accounting. Among others were John Wingert, Bill Small, Gresh Brebach and many more. (I was saddened to lose one of our classmates Wayne Pearson ‘61, who was shot down in his F-4 in 1967, just before my carrier group arrived in Southeast Asia.)
Who do you stay in touch with now?
John Wingert and I had lunch together a couple of weeks ago, because he lives here in San Diego. Most of my ATO friends are in the Midwest so Betty and I see them very infrequently. Even when we’re there, we’re usually visiting her sisters and our brothers in law. We’ll try to do a better job of staying in touch in the future, over and above Christmas cards.
Tell us about your family, where you are living and what you do for fun now?
Our daughter Kem and her husband, Philip Graham and their four children live only a few miles from us. Brock (18), Gunner (16) had excellent football seasons. Their twin sisters, Margot and Marianne (14) are volleyball players, so between football and volleyball, our weekends are pretty absorbed with sports.
About 4 years ago, Betty received Univ. of Illinois’ Humanitarian award for her founding of a non-profit, United Through Reading (UTR). When I got back from Vietnam, Kem was 2 years old and did not recognize me. Betty decided to fix that problem for returning military personnel and founded UTR whereby deployed parents read their children’s favorite bedtime stories on DVD so the child can recognizes the parent upon their return. The program is now on every Navy ship as well as all Army, Air Force and Marine facilities. They have accumulated almost 2 million beneficiaries. She retired from UTR 3 years ago and now I help her take the Reading Legacies program into jails and prisons to benefit the children of the incarcerated, whom we consider to be the most vulnerable children in our society. Between Reading Legacies and our extended family’s activities– that’s what we do.
bmohlenbrock@verras.com
858.354.0415